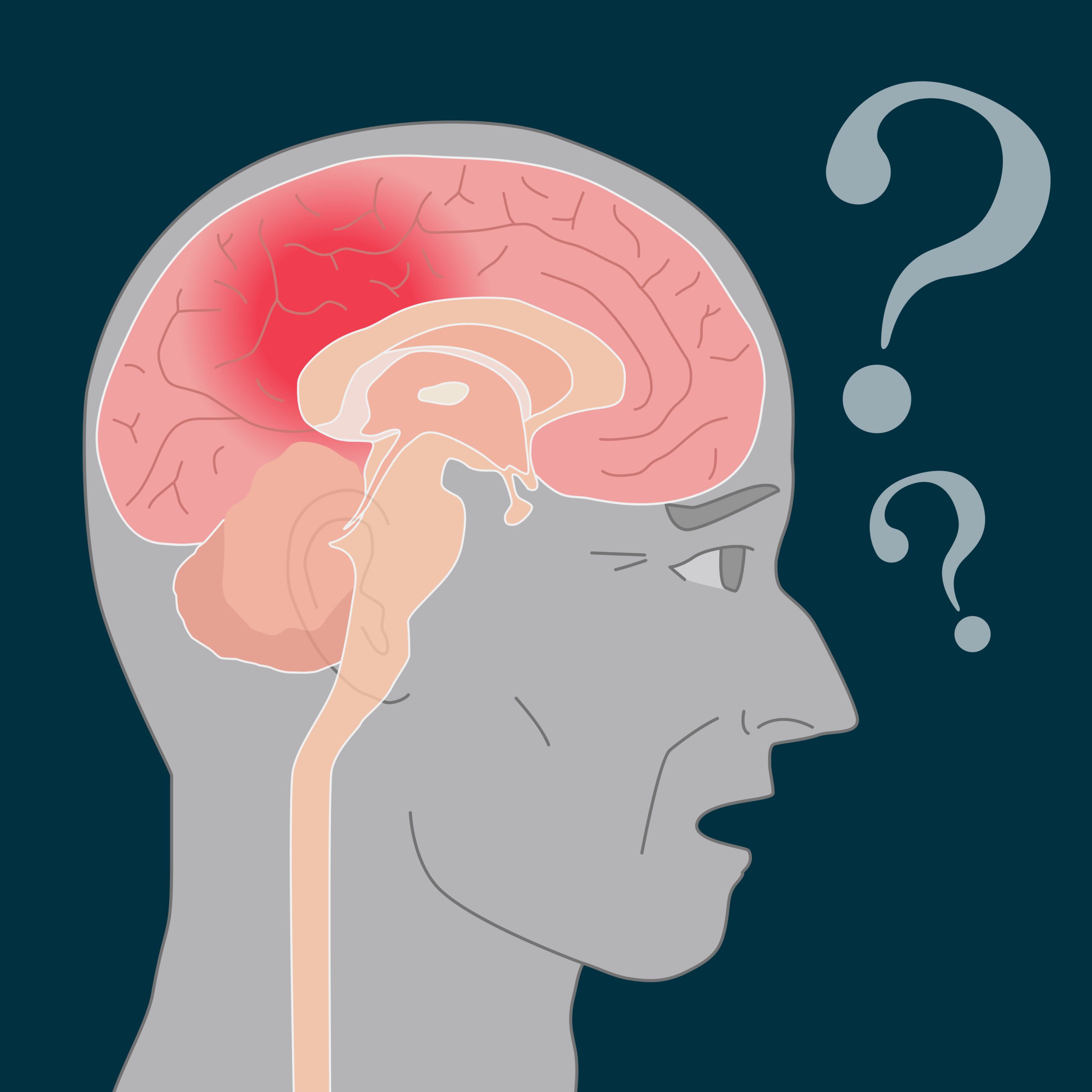
Frontotemporal dementia, also known as frontotemporal lobar degeneration, is a type of dementia that affects the frontal and temporal lobes of the brain. These lobes are responsible for many functions, including language, behavior, and decision-making. Frontotemporal dementia is characterized by a decline in these cognitive and behavioral abilities, which can significantly impact a person’s quality of life.
Causes and Risk Factors
Frontotemporal dementia is caused by the degeneration or death of nerve cells in the frontal and temporal lobes of the brain. Various factors, including genetics, environmental exposures, and underlying medical conditions, can cause this degeneration.
One of the most common causes of frontotemporal dementia is a genetic mutation that leads to the accumulation of abnormal proteins in the brain. These proteins, called tau and TDP-43, can cause damage to nerve cells and lead to their death.
Environmental factors, such as exposure to toxins or traumatic brain injury, may also increase the risk of frontotemporal dementia. Additionally, certain medical conditions, such as HIV/AIDS or multiple sclerosis, can increase the risk of frontotemporal dementia.
Symptoms of Frontotemporal dementia
Frontotemporal dementia can present with a wide range of symptoms, depending on the affected area of the brain.
One of the most common symptoms of frontotemporal dementia is a decline in language abilities. This can include difficulty speaking, understanding language, or using language to communicate. In some cases, individuals with frontotemporal dementia may also have trouble with reading and writing.
Frontotemporal dementia can also cause changes in behavior and personality. These changes can include a loss of empathy, impulsivity, disinhibition, and apathy. These changes can significantly impact a person’s social interactions and relationships.
Other symptoms of frontotemporal dementia may include:
- The decline in language abilities, such as difficulty speaking, understanding language, or using language to communicate
- Changes in behavior and personality, including a loss of empathy, impulsivity, disinhibition, and apathy
- Memory loss
- Difficulty with planning and organization
- The decline in problem-solving skills
- Loss of interest in previously enjoyed activities
- Difficulty with decision-making
- Changes in social behavior, such as becoming more isolated or exhibiting inappropriate social behaviors
- Decreased motivation and drive
- Loss of ability to initiate or complete tasks.
Diagnosis
A team of healthcare professionals, including a neurologist, a neuropsychologist, and a speech-language pathologist, typically diagnoses frontotemporal dementia. The diagnostic process typically involves a thorough evaluation of the individual’s medical history, a physical examination, and a series of tests to assess cognitive and behavioral function.
The most commonly used tool for diagnosing frontotemporal dementia is the Mini-Mental State Examination (MMSE). This test is a brief assessment of cognitive function that includes questions about memory, orientation, language, and other cognitive abilities.
Other tests that may be used to diagnose frontotemporal dementia include brain imaging scans, such as magnetic resonance imaging (MRI) or computed tomography (CT), and genetic testing to identify.
1. Early-stage Frontotemporal dementia
During the early stage of frontotemporal dementia, individuals may experience subtle changes in behavior and personality. They may need help with planning and organization and may need help with decision-making and problem-solving. They may also experience changes in their social behavior, such as becoming more impulsive or showing less empathy toward others.
2. Middle-stage
As frontotemporal dementia progresses to the middle stage, cognitive and behavioral changes become more pronounced. Individuals may need help with language, either speaking or understanding it. They may have difficulty with memory and may have trouble completing familiar tasks. They may also show significant changes in their personality, such as becoming more apathetic or disinhibited.
3. Late stage
In the late stage of frontotemporal dementia, individuals may have severe difficulty with communication and may be unable to speak or understand language. They may also have significant memory loss and require assistance with daily activities, such as bathing and dressing. They may become more dependent on caregivers and may need round-the-clock supervision.
4. End-stage
A severe decline in cognitive and physical functioning marks the end stage of frontotemporal dementia. Individuals may lose the ability to walk and may be unable to communicate or interact with others. They may also experience changes in their sleep patterns and difficulty swallowing.
5. Early onset
Frontotemporal dementia can occur at any age, but it is most commonly diagnosed in people in their 50s and 60s. When it occurs in individuals under 60, it is referred to as early-onset frontotemporal dementia.
6. Behavioral variant frontotemporal dementia (bvFTD)
Behavioral variant frontotemporal dementia, also known as bvFTD, is a subtype of frontotemporal dementia characterized by changes in behavior and personality. Individuals with bvFTD may become more impulsive, disinhibited, or apathetic and have difficulty with social interactions.
7. Primary progressive aphasia (PPA)
Primary progressive aphasia, or PPA, is a subtype of frontotemporal dementia characterized by a decline in language abilities. Individuals with PPA may have difficulty speaking, understanding language, or using language to communicate. They may also need help with reading and writing.
Home Care Near Me. Let’s Get Started!
Get Immediate Help with Information, Costs & Payment Options.